Sleep Apnea and Snoring Surgeries
Snoring is more than just a loud noise at night. In many people, it is a sign that the airway has become too narrow during sleep. In some cases this narrowing is so severe that breathing repeatedly stops for a few seconds at a time, a condition known as sleep apnea. These pauses in breathing can lead to poor sleep quality, daytime tiredness, concentration problems, morning headaches and long-term strain on the heart and blood vessels. As an Otolaryngologist (ENT Specialist), Dr. Mustafa Çakır evaluates snoring and suspected sleep apnea in detail and, when appropriate, offers surgical solutions to open the airway and improve breathing during sleep.
Uyku Apnesi ve Horlama Cerrahileri
Doctor Mustafa Clinic
Uyku Apnesi ve Horlama Cerrahileri
Snoring is more than just a loud noise at night. In many people, it is a sign that the airway has become too narrow during sleep. In some cases this narrowing is so severe that breathing repeatedly stops for a few seconds at a time, a condition known as sleep apnea. These pauses in breathing can lead to poor sleep quality, daytime tiredness, concentration problems, morning headaches and long-term strain on the heart and blood vessels. As an Otolaryngologist (ENT Specialist), Dr. Mustafa Çakır evaluates snoring and suspected sleep apnea in detail and, when appropriate, offers surgical solutions to open the airway and improve breathing during sleep.
Snoring and Sleep Apnea – What’s the Difference?
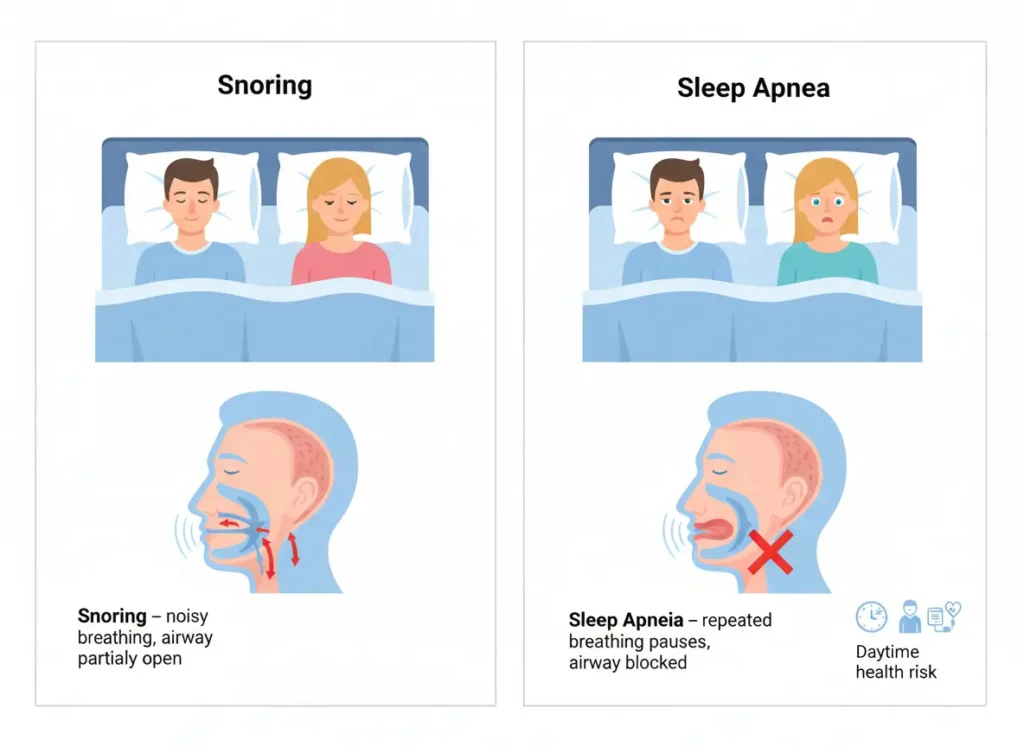
Snoring occurs when air passes through a narrowed upper airway and causes soft tissues in the nose, soft palate, uvula or throat to vibrate. Many people snore occasionally without any serious health problem. However, when snoring is loud, frequent and accompanied by breathing pauses, choking or gasping at night, it may indicate obstructive sleep apnea.
In obstructive sleep apnea, the airway repeatedly collapses or becomes blocked during sleep. The brain briefly wakes the person up just enough to reopen the airway, often without them fully remembering it. This cycle can repeat many times per hour, fragmenting sleep and reducing oxygen levels. Over time, untreated sleep apnea can contribute to high blood pressure, heart disease, stroke, diabetes, weight gain and mood disorders, as well as reduced performance at work and increased risk of traffic or work accidents due to daytime sleepiness.
When to Seek Evaluation
You should consider an evaluation with an ENT specialist if you or a family member experience symptoms such as very loud, habitual snoring that disturbs others; pauses in breathing observed by a partner, often followed by choking or gasping; waking up unrefreshed, with morning headaches or dry mouth; excessive daytime sleepiness, difficulty concentrating or falling asleep easily while reading, watching TV or driving; and, in children, snoring with restless sleep, mouth breathing, growth issues or behavior and attention problems.
Because snoring and sleep apnea can involve the nose, soft palate, tonsils, tongue base and other structures, a careful examination is essential to identify which areas are contributing most to the obstruction.

ENT Assessment with Dr. Mustafa Çakır
The evaluation begins with a detailed discussion of your symptoms. Dr. Mustafa Çakır asks about the pattern and duration of snoring, any witnessed apnea episodes, the quality of your sleep, how you feel during the day, weight changes, medications, other medical conditions and family history. For children, information from parents or caregivers about sleep behavior and school performance is very important.
A thorough ENT examination follows, including the nose, oral cavity, throat and neck. The size of the tonsils, the length and position of the soft palate and uvula, the tongue base, the nasal passages and the possible presence of adenoid tissue or nasal obstruction are evaluated. In many cases, a sleep study (polysomnography) is recommended in cooperation with a sleep center to objectively measure how severe sleep apnea is and how often breathing stops during the night.
Based on these findings, Dr. Çakır explains whether the problem is simple snoring, mild to moderate sleep apnea or more severe disease, and which treatment options are suitable.

Non-Surgical and First-Line Treatments
Surgery is not the first step for every patient. For many people with mild symptoms, lifestyle modifications can have a strong impact. These include weight loss in overweight patients, avoiding alcohol and sedative medications before bedtime, changing sleep position (for example avoiding sleeping on the back) and treating nasal obstruction with appropriate medical or surgical therapy when necessary.
For moderate to severe sleep apnea, especially when there are significant health risks, CPAP (continuous positive airway pressure) therapy is often considered the gold standard. This involves wearing a mask connected to a machine that gently delivers air pressure to keep the airway open during sleep. Some patients also benefit from specially designed oral appliances that reposition the jaw and tongue. Even when surgery is being considered, these non-surgical approaches are part of the global treatment plan and may be used before or after an operation.
Surgical Options for Snoring and Sleep Apnea
When structural problems in the nose and throat significantly contribute to snoring or obstructive sleep apnea, and when non-surgical measures are not sufficient or not tolerated, surgical treatment may be recommended. The choice of procedure depends on which parts of the airway are narrowed.
If nasal obstruction plays a major role, procedures such as septoplasty for a deviated septum or turbinate surgery to reduce swollen nasal tissues can improve airflow and may reduce snoring or enhance tolerance to CPAP.
In patients with enlarged tonsils, particularly in children and younger adults, tonsillectomy (removal of the tonsils) and sometimes adenoidectomy can greatly enlarge the airway behind the palate and tongue, often leading to a marked improvement in snoring and sleep apnea.
For soft palate and uvula–related obstruction, palate surgeries may be considered. These procedures, using various modern techniques, aim to tighten or reshape the soft palate and reduce vibration, helping both snoring and airway patency. In selected cases with more complex multilevel obstruction, additional procedures at the tongue base or other regions may be discussed as part of a staged or combined approach.
Dr. Mustafa Çakır carefully selects surgical candidates, taking into account the severity of sleep apnea, airway anatomy, general health, previous treatments and patient expectations. The goal is always to improve airflow in a durable, safe way while minimizing complications.
Surgery and Recovery
Sleep apnea and snoring surgeries are typically performed under general anesthesia in a hospital setting. The exact duration of surgery and the length of hospital stay depend on which procedures are being carried out. For example, isolated nasal surgery may be a short, same-day procedure, while combined tonsil and palate surgeries may require overnight observation.
After surgery, patients may experience throat pain, difficulty swallowing, changes in voice, nasal congestion or mild bleeding, depending on the type of operation. Pain medication, adequate hydration and a gradual return to normal eating are important parts of recovery. For children, parents receive clear instructions on diet, activity and warning signs. Adults may need to take time off work and avoid strenuous activity for a recommended period.
Swelling and healing changes can affect the airway temporarily, so final improvement in snoring and sleep quality may take several weeks to become fully apparent. Follow-up visits with Dr. Mustafa Çakır are essential to monitor healing, manage any discomfort and assess the effect of surgery on symptoms.
Results and Expectations
Surgery for snoring and sleep apnea can significantly reduce or eliminate loud snoring, improve nighttime breathing and reduce daytime sleepiness in selected patients. However, results vary depending on the severity of disease, the specific anatomy of the airway and lifestyle factors such as weight and sleep habits.
In some cases, surgery is part of a combined treatment plan rather than a complete replacement for other therapies. For instance, nasal or throat surgery may be performed to make CPAP treatment more comfortable and effective or to reduce snoring while still using other methods to manage underlying sleep apnea. Dr. Mustafa Çakır emphasizes realistic expectations and explains in advance what level of improvement is likely and what additional steps may be needed after surgery.

A Comprehensive Approach to Better Sleep
Snoring and sleep apnea affect not only the person who has them, but also their partner, family life, work performance and long-term health. For this reason, Dr. Mustafa Çakır takes a comprehensive, step-by-step approach: accurate diagnosis, optimization of non-surgical treatments, and thoughtfully selected surgical interventions when needed.
The overall aim is to provide quieter, more regular breathing during sleep, deeper rest at night, more energy during the day and better protection for the heart and brain over the long term. With a structured, personalized plan, many patients experience a profound improvement in their quality of life and in the wellbeing of those around them.